Polycystic Ovary Syndrome
Polycystic Ovary Syndrome (PCOS) is the most common endocrinopathy affecting reproductive-aged women with a prevalence of 8–13%. It is characterized by ovulatory dysfunction and causes menstrual dysfunction, hyperandrogenism, and polycystic ovaries.
Two out of three of the following criteria are required to make the diagnosis:
- Oligomenorrhea: Irregular periods with intervals between menstrual cycles of more than 35 days and/or less than nine periods per year.
- Clinical or biochemical signs of hyperandrogenism
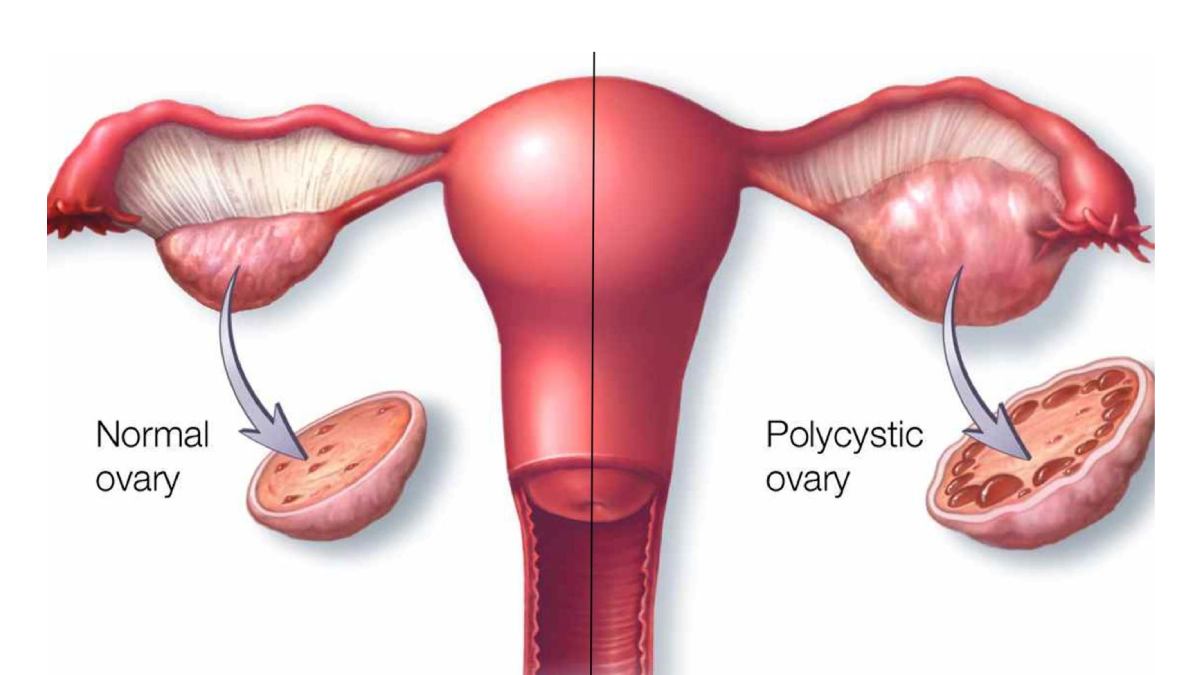
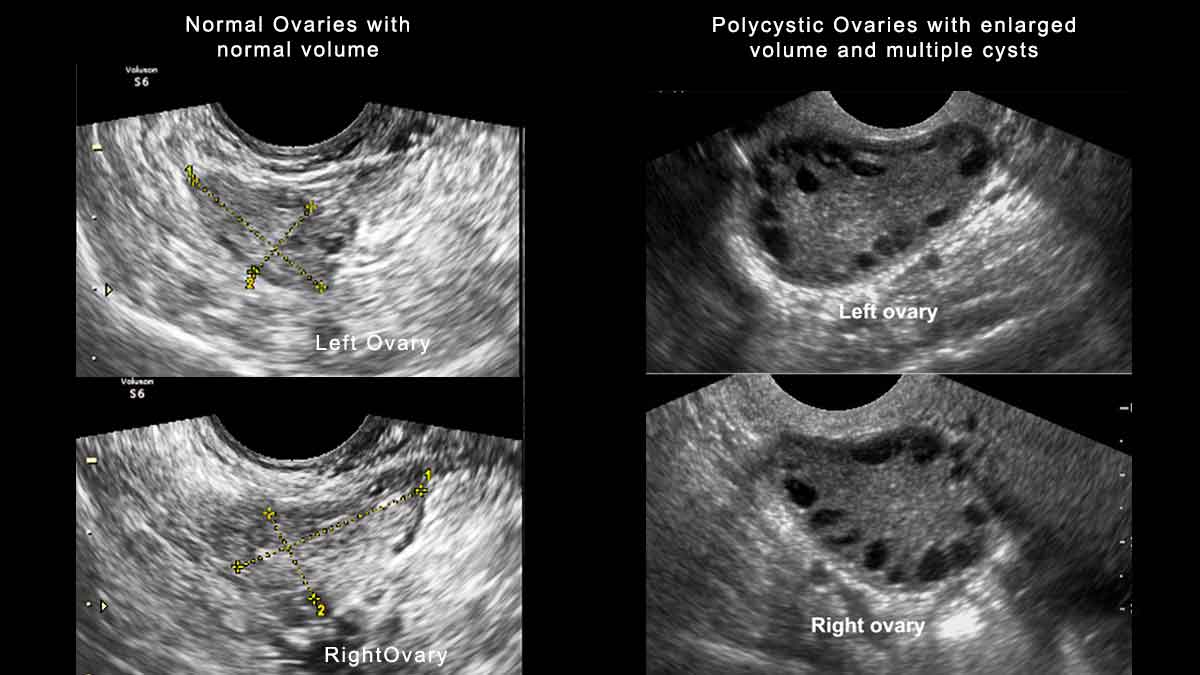
- Polycystic ovaries
What Causes PCOS?
PCOS is an extremely heterogenetic and complex disease. PCOS may be related to many different factors working together. These are insulin resistance, increased levels of hormones called androgens, and an irregular menstrual cycle.
Is Having Polycystic Ovary Always a Problem?
The typical polycystic appearance of the ovaries is seen on a transvaginal ultrasound in the majority of women with irregular menses and hyperandrogenism. However, this ultrasound appearance is not specific, it may be seen in women with regular menstruation. Ultrasound criteria include the presence of 12 or more follicles in each ovary measuring 2 to 9 mm in diameter or increased ovarian volume (>10ml). For many women, the diagnosis of ovarian cysts raises a concern about tumors but they are numerous small eggs that are not ovulating.
Menstrual Dysfunction
Women with PCOS show menstrual irregularities that range from oligomenorrhea and amenorrhea to very heavy, irregular periods. The menstrual irregularity typically begins in the peripubertal period and menarche may be delayed. After age 40 years, women with PCOS often have regular cycles.
Hyperandrogenism
Acne, hirsutism, and male pattern hair loss are clinical signs. In this elevated serum androgen concentrations are found. Hirsutism is excessive hair growth in male distribution (upper lip, chin, periareolar area, mid sternum, along the linea alba of the lower abdomen)
Obesity
40 to 85 percent of women with PCOS are overweight. There is a high prevalence of insulin resistance.
Complications of PCOS

- Type 2 diabetes
- Obesity
- Infertility
- Gestational diabetes
- Miscarriage or premature birth
- Metabolic syndrome
- Cardiovascular disease
- Sleep apnea
- Depression, anxiety and eating disorders
- Abnormal uterine bleeding
- Endometrial cancer
If you observe any of the above symptoms, visit your gynecologist without any delay.
TREATMENT
- Lifestyle changes: A low glycemic index and an anti-inflammatory diet are recommended.

- Weight loss: At least 5 to 10 percent reduction in body weight will improve the likelihood of ovulation and conception.

- Exercise
- Combined estrogen-progestin contraceptives: COCs are used for androgen suppression and menstrual cycle control.
- Spironolactone: Anti-androgen therapy can reduce the growth of terminal hair.
- Metformin: The drug decreases hepatic glucose production and intestinal absorption of glucose. Also, it reduces the need for insulin secretion so metformin is associated with an improvement in glucose levels.
- Bariatric surgery
- Laparoscopic ovarian surgery
- Ovulation induction
- IVF
REFERENCES
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5301909/
https://www.uptodate.com/contents/diagnosis-of-polycystic-ovary-syndrome-in-adults
https://www.fertstert.org/action/showPdf?pii=S0015-0282%2818%2930400-X
https://pubmed.ncbi.nlm.nih.gov/26509855/
https://www.acog.org/patient-resources/faqs/gynecologic-problems/polycystic-ovary-syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935309/