✨Book online and enjoy a 5% discount on your first consultation
Home » Gynecology Services » Pelvic Floor Disorders
Medical Service Name – Pelvic Floor Disorders
Pelvic floor dysfunction is one of the most frequent female-specific disorders. According to statistics, at least one-third of all women experience pelvic floor dysfunction at some point in their lives. Pelvic floor muscle dysfunction develops as women age.
Possible Causes
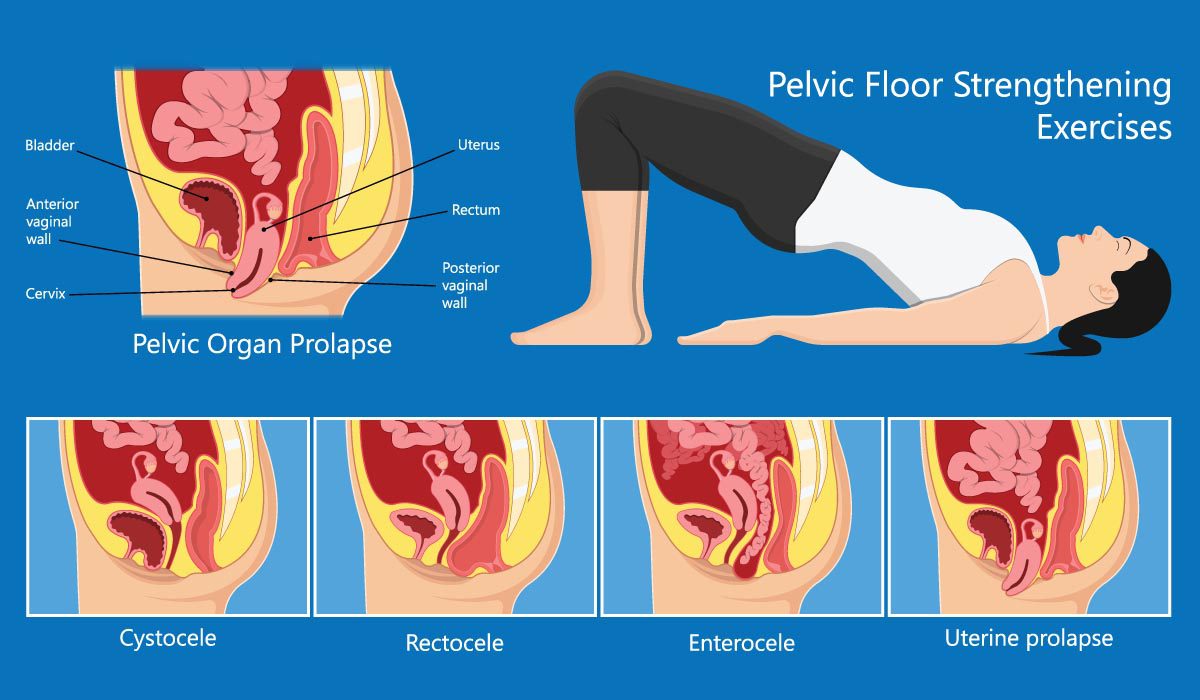
The uterus, cervix, vagina, bladder, bowel, urethra, small intestine, and rectum are all held in place by the pelvic floor, which is a network of muscles and tissues that works like a hammock. The disease arises when these pelvic muscles are strained as a result of a tear or loosening.
Pelvic floor disorders are more common in older persons, particularly women, whose bodies have degenerated and have given birth naturally.
Risk Factor
Sign & Symptoms
Diagnosis
Typically, our team of expert doctors will begin by inquiring about your symptoms and collecting a thorough medical history. The following are some of the questions we may ask you:
We may perform a physical exam to assess your ability to regulate your pelvic floor muscles. Our doctors will examine these muscles for spasms, knots, or weakness with their hands. They may also need to do an intrarectal (rectum) or vaginal exam on you.
Other tests may be administered to you, such as:
Treatment Options at 7DMC
Weak muscles may be strengthened and made to operate correctly again by exercising them regularly over time. Walking or other mild exercises might also assist in strengthening your pelvic floor muscles.
If symptoms of pelvic floor dysfunction (such as an overactive bladder) aren’t addressed, they tend to persist or worsen. Instead of suffering from pain and discomfort, a consultation with your provider may frequently help you better your daily life.
Sit in a comfortable position with your weight equally distributed between your sitting bones. Cross your legs as little as possible. Your feet should be supported on the ground (or on a tiny footstool if necessary), and your hips should be at a 90-degree angle.
Near Dubai Miracle Garden,
Diamond Business centre A,
1st Floor,
Arjan, AI Barsha,
Dubai.
Career@7DMC | Privacy Policy | Patient Data
WhatsApp us